By Dr. Brandon Rieders, Gastroenterologist
When we think about health, we often focus on diet, exercise, or sleep. But the real powerhouse of your well-being lies within your gastrointestinal (GI) tract. This complex system—from your mouth to your colon—not only digests food, but also nourishes your immune system, regulates inflammation, and even impacts your mood through the gut-brain axis.
Let’s explore how the GI tract works, how it shapes your health, and what you can do to keep it running smoothly.
What Is the GI Tract and How Does It Support Gut Health?
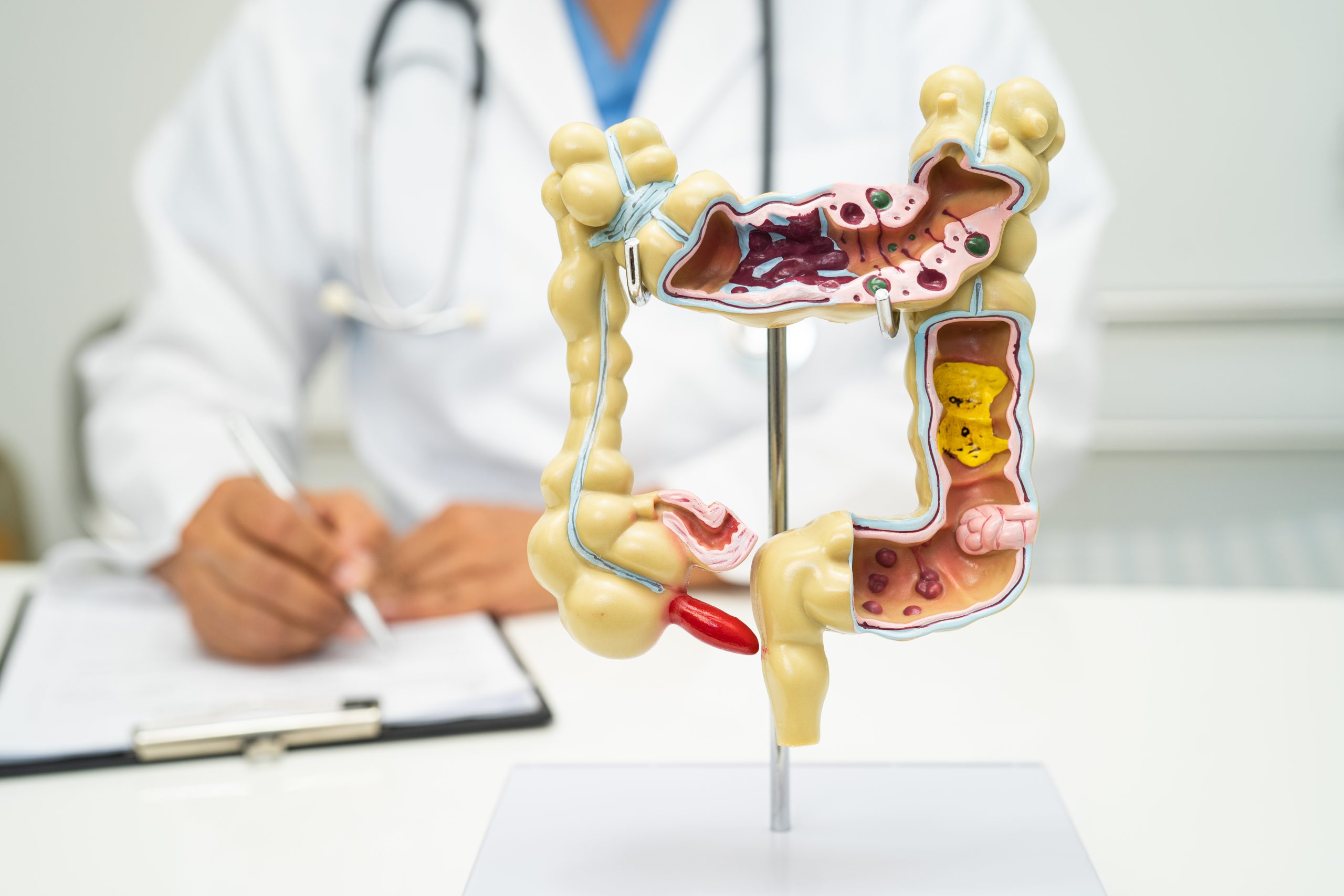
The GI tract is a long, interconnected system made up of the mouth, esophagus, stomach, small intestine, large intestine (colon), rectum, and anus. Each section has a specialized role:
- Breaks down food so nutrients can be absorbed
- Processes and eliminates waste
- Supports a diverse microbial ecosystem
- Communicates with the immune and nervous systems
This system is home to trillions of microbes—collectively known as the gut microbiome—that play a critical role in digestion, immunity, metabolism, and even mental health [1].
Main Sections of the GI Tract (and Their Role in Gut Health)
1. Mouth
Digestion begins here. Enzymes in saliva (like amylase) start breaking down carbohydrates. Proper chewing increases surface area and improves microbial accessibility further down the tract.
2. Esophagus
This muscular tube transports food from your mouth to your stomach via peristalsis (wave-like muscle contractions). Healthy motility here reduces the risk of reflux and esophageal irritation.
3. Stomach
A key digestive chamber where acid (HCl) and enzymes break down proteins. Maintaining the right pH is essential—not only for digestion, but also for controlling microbial populations and preventing infection.
4. Small Intestine
The workhorse of nutrient absorption. It interacts with bile (from the liver), enzymes (from the pancreas), and hormones to break down fats, proteins, and carbohydrates. It also plays a key role in immune defense and hosts some beneficial microbes.
5. Large Intestine (Colon)
This is where the majority of your gut microbes live. They ferment fibers into short-chain fatty acids (SCFAs), which reduce inflammation, support immunity, and even influence mood [2].
6. Rectum and Anus
These final sections store and eliminate stool. Regular, healthy bowel movements are one of the best signs of a well-functioning gut.
The Gut Microbiome: The Heart of Gut Health
The gut microbiome refers to the trillions of bacteria, viruses, and fungi that live in your digestive tract—primarily in the colon. These microbes:
- Help digest fibers and resistant starches
- Produce vitamins like B12 and K
- Regulate the immune system
- Influence hormone and neurotransmitter production (like serotonin)
However, microbial balance can be disrupted by poor diet, chronic stress, medications (especially antibiotics), and lack of sleep [3].
When this balance is thrown off, it can lead to symptoms like bloating, fatigue, brain fog, or even more serious GI conditions.
Common GI Tract Conditions That Affect Gut Health
Many chronic health conditions are rooted in dysfunction within the GI tract:
- IBS (Irritable Bowel Syndrome): Often linked to dysbiosis (microbial imbalance) and gut hypersensitivity
- IBD (Crohn’s & Ulcerative Colitis): Autoimmune inflammation of the GI tract
- Leaky Gut (Increased Intestinal Permeability): A compromised gut lining that allows toxins and bacteria to escape into the bloodstream
- GERD, bloating, constipation, diarrhea: Often signs of an imbalanced microbiome or sluggish digestion
In these cases, gut-targeted strategies—like dietary fiber, probiotics, stress management, or gut-calming botanicals—can make a measurable difference.
How to Support Gut Health Through the GI Tract
Your daily habits have the power to strengthen or stress your GI system. Here’s what I recommend to patients:
- Eat a diverse, plant-forward diet rich in fiber to nourish beneficial bacteria
- Include both probiotics and prebiotics through foods and, if needed, supplements
- Stay hydrated to support motility and stool formation
- Limit ultra-processed foods and alcohol that irritate the gut lining
- Avoid unnecessary antibiotics which can wipe out good microbes
- Manage stress and prioritize sleep, which help regulate the gut-brain connection
Many patients also benefit from natural gut-supporting ingredients like peppermint, ginger, artichoke leaf, and digestive enzymes—like those found in comprehensive blends such as Happitum™. These help relieve bloating, support digestion, and promote gut comfort.
The Gut-Brain Connection
The gut-brain axis is the two-way communication between your digestive system and central nervous system. Your gut is lined with over 100 million neurons and produces 90% of the body’s serotonin, a neurotransmitter that affects mood, sleep, and appetite [4].
That means stress can disrupt digestion—and poor digestion can affect your mental health. Supporting a healthy gut often results in benefits that extend far beyond the digestive tract.
Conclusion
Your GI tract isn’t just a food processor—it’s your immune fortress, your microbial metropolis, and a key player in mood regulation. When it’s working well, everything from your energy to your skin to your stress levels feels better.
Nurture it with the right foods, healthy habits, and support when needed. Happitum™ contains ashwagandha and theanine, toning the gut-brain axis and providing both gut calming and mental calming. It helps balance cortisol levels and calm the Vagus nerve, so during times of stress your stomach butterflies don’t become overwhelming. A well-fed, well-functioning gut truly is the foundation of total body wellness.
References
[1] Thursby, E., & Juge, N. (2017). Introduction to the human gut microbiota. Biochemical Journal, 474(11), 1823–1836.
[2] Koh, A., De Vadder, F., Kovatcheva-Datchary, P., & Bäckhed, F. (2016). From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites. Cell, 165(6), 1332–1345.
[3] Zmora, N., Suez, J., & Elinav, E. (2019). You are what you eat: diet, health and the gut microbiota. Nature Reviews Gastroenterology & Hepatology, 16, 35–56.
[4] Carabotti, M., Scirocco, A., Maselli, M. A., & Severi, C. (2015). The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Annals of Gastroenterology, 28(2), 203–209.